Recent peer-reviewed research conducted in Turkey investigated whether the Pfizer-BioNTech (BNT162b2) mRNA COVID-19 vaccine has short-term effects on the cornea, focusing specifically on the corneal endothelium. This innermost layer of the cornea plays a critical role in maintaining transparency, hydration, and proper visual function. Unlike sensationalized claims circulating online, the study does not suggest that the vaccine causes vision loss or eye disease in healthy individuals. Instead, it represents a careful scientific effort to measure subtle cellular changes that could occur after vaccination, using advanced ophthalmologic imaging techniques. By exploring this underexamined aspect of vaccine safety, the research contributes to ongoing monitoring without implying any clinical harm. The authors are explicit that their findings should not discourage vaccination, emphasizing that COVID-19 vaccines remain both safe and essential for public health protection, while adding to the scientific understanding of how the body responds to immunization.
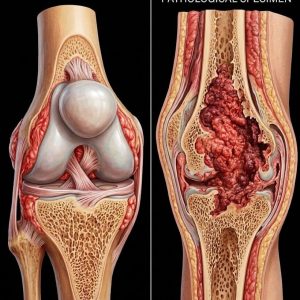
The study recruited 64 adult participants, all of whom had no pre-existing ocular disease. Each participant underwent a comprehensive eye examination before receiving the first vaccine dose and again approximately two months after completing the second dose. Researchers measured several key indicators of corneal health: corneal thickness, endothelial cell density (the number of cells per square millimeter), variation in cell size (polymegathism), and variation in cell shape (pleomorphism). These measurements are standard in ophthalmology, particularly for assessing corneal readiness before surgeries such as cataract extraction or corneal transplantation. Following vaccination, subtle changes were observed: a minor increase in average corneal thickness, an approximate 8% decrease in endothelial cell density, and slight increases in the variability of cell size and shape. While these changes were detectable via imaging, they were entirely subclinical—meaning participants experienced no symptoms, functional impairments, or visual disturbances.
Importantly, all measured parameters remained well within normal, clinically safe ranges for individuals with healthy eyes. None of the participants reported blurred vision, eye pain, swelling, or reduced visual acuity throughout the study period. The researchers emphasized that a slow, natural decline in corneal endothelial cells occurs with age, and the observed changes after vaccination did not exceed thresholds associated with corneal dysfunction or disease. In other words, the alterations were measurable but not functionally significant. Participants’ vision remained fully intact, and no medical treatment was necessary. These findings underscore that the study does not provide evidence of eye damage, blindness, or permanent harm from the Pfizer vaccine in people without pre-existing ocular issues. Instead, it demonstrates the rigorous, cautious monitoring scientists undertake to ensure vaccine safety across multiple physiological systems.
While the study’s results reassure the general population, the researchers noted that corneal endothelial cells do not regenerate. This biological principle is why ophthalmologists monitor these cells in patients at higher risk, such as those who have undergone cataract surgery, corneal transplantation, or who suffer from chronic corneal disease, prior infections, or inflammatory eye conditions. In such cases, even a minor reduction in endothelial cell density could theoretically have greater clinical significance. The authors are careful to clarify that the study does not establish harm in these groups; rather, it highlights a need for continued vigilance and individualized assessment. Eye specialists may consider the data when evaluating patients with pre-existing vulnerabilities, ensuring that any potential changes are identified and managed appropriately, though for the vast majority of people, vaccination presents no ocular risk.
The study’s limitations are equally important to consider. The sample size was modest, the follow-up period relatively short, and participants with known eye disease were excluded. Consequently, the findings cannot be extrapolated to long-term effects, repeated booster doses, or rare complications. The researchers explicitly called for larger, longer-term studies to determine whether the observed corneal changes are temporary, stable, or reversible over time. They also cautioned against misinterpretation of the data, reiterating that there is no evidence of causation, no indication of clinical damage, and no reason to reconsider the broad recommendation for COVID-19 vaccination. The study is a demonstration of ongoing scientific observation, illustrating how researchers carefully track subtle physiological effects without generating unwarranted alarm or misinformation.
In conclusion, this peer-reviewed research confirms that minor, measurable changes in the corneal endothelium may occur after Pfizer COVID-19 vaccination, but these effects are subclinical and do not impact vision or ocular health in healthy adults. All results remained within normal safety margins, and participants experienced no functional consequences. For the general population, there is no cause for concern, and the findings reinforce the safety of COVID-19 vaccines. For individuals with pre-existing corneal conditions, routine ophthalmologic care remains important, though vaccination itself is not contraindicated. Overall, the study highlights the value of ongoing scientific vigilance, confirming that COVID-19 vaccines are not only life-saving in preventing severe disease and hospitalization, but also safe for ocular health. The research serves as an example of careful, evidence-based monitoring rather than a signal of risk.